


A 14-year-old girl presented to the endocrine department for evaluation of primary amenorrhea. Her medical history was remarkable for recurrent abdominal pain and diarrhea since infancy, with growth in the third percentile for weight and height. Physical examination revealed “bumpy lips” (Figure 1; available at www.jpeds.com), diastema of her anterior teeth, and several lesions on the tip of the tongue and on the oral mucosa (Figure 2 and Figure 3), suggesting the presence of multiple mucosal/submucosal neuromas. The patient had a Marfanoid habitus with slight ligamentous laxity and clinodactyly of 1 finger. Laterocervical lymph nodes were palpable bilaterally without enlargement of the thyroid.
diagnosis??? complications? therapy?- ¿?

A 16-day-old white female infant was admitted to the pediatric emergency room for the acute onset of a widespread vesiculopustular eruption on her trunk without evident systemic symptoms.
The baby was born after spontaneous delivery at 40 gestational weeks with a birth body weight of 3,145 g. Apgar scores were 10 and 10 at the first and fifth minutes, respectively, and all neonatal metabolic screenings were normal. The mother was in healthy conditions at the moment of delivery and had no family history of hereditary and systemic diseases.
Upon physical examination, the patient was lively and reactive, the anterior fontanelle was normotensive, the muscle tone and neonatal reflexes were normal, and body temperature was 35.6 °C. Vital signs were as follows, heart rate was 132 beats/min, respiratory rate was 48/min, and blood pressure was 64/32 mmHg. Hearts beats were regular, without murmur, and breathing sounds were clear. Neurological findings were negative, and cerebral ultrasound did not reveal abnormalities.
The skin of her anterior trunk surface was entirely covered by a myriad of yellow pustules of different sizes, without surrounding erythema. The lesions appeared to be non-follicular and were isolated on the upper part of the trunk and mostly confluent in large pustules over the abdominal area (Fig. 1). No mucosal involvement was detected, and genitals were spared too.
Septic work-up was immediately performed,and a specimen of pustule fluid was obtained for cultural examination. In the meantime, an intravenous empirical therapy with oxacillin and gentamicin was introduced, suspecting an infectious etiology.
Laboratory findings showed no abnormalities; in particular, there was no leucocytosis, and inflammatory parameters were negative. The other routine laboratory results were all within reference range, and autoimmunity profile was negative too. Serological examinations of herpes infection, cytomegalovirus, rubella, toxoplasmosis, and syphilis were also negative.
Gram stains of the pustular content showed no bacteria. Bacterial, viral, and fungal cultures were all sterile, including the blood and pus cultures. Systemic antibiotic therapy was therefore discontinued.
We decided to perform a cytologic examination of vesicular fluid with Wright's stain. Cytodiagnosis confirmed the absence of multinucleated giant cells and revealed a predominance of polymorphic neutrophils (>80 %) over eosinophils (<20 %) in the cellularity.
Two biopsy specimens were obtained using a 4-mm punch biopsy for histological examination and immunofluorescence studies.
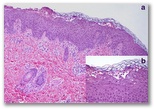
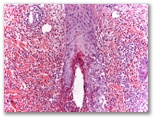
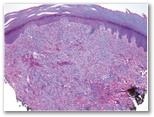
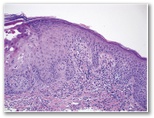
Histological examination revealed subcorneal microvesicles, containing acantholytic and dyskeratotic keratinocytes, red blood cells, neutrophils, and occasional eosinophils; hyperkeratosis, parakeratosis, and superficial perivascular dermatitis with scanty lymphohistiocytic inflammatory infiltrates, and few interstitial neutrophils and eosinophils were also detectable (Fig. 2a, b). Direct immunofluorescence studies using antibodies to IgG, IgA, IgM, and fibrinogen proved negative.- erythema toxicum neonatorum
- infantile acropustulosis
- pustular miliaria
- Langerhans cells hystiocytosis
- incontinentia pigmenti.
- Transient neonatal pustular melanosis

A 7‐month‐old, full‐term boy presented with a history of recurrent and self‐limiting episodes of pruritic pustules on the scalp that had occurred since the first day of life. He was otherwise healthy, and his birth had been unremarkable. Outbreaks usually occurred every month and lasted for approximately one week. No fever, weight loss, or alteration in feeding were reported. The infant had been treated with systemic antibiotics, such as amoxicillin–clavulanic acid and cloxacillin, for a possible infectious etiology with no response. Topical mupirocin, corticosteroids, and ciclopirox olamina had been previously used with transitory improvement.
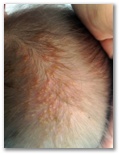
Clinical examination revealed confluent, slightly exudative pustules surrounded by erythema with yellow crusting located on the scalp (Fig. 1). The hair appeared agglutinated by the exudate. Cultures for bacteria and fungi were negative.
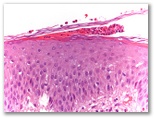
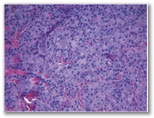
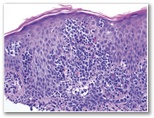
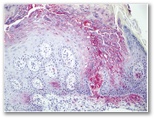
At the patient's second visit, a biopsy specimen was obtained from his scalp. Histopathologic examination showed an inflammatory infiltrate in the entire thickness of the dermis (Fig. 2). A subcorneal pustule containing eosinophils was also observed (Fig. 3). The hypodermis was seen to be involved. The reticular dermis showed a strong eosinophilic peri‐ and intrafollicular infiltrate- scalp pyoderma
- Eosinophilic pustular folliculitis of infancy
- incontinentia pigmenti
- Acropustulosis of infancy


A healthy teenage girl was referred by Rheumatology regarding papules and nodules on the hands in the setting of arthritis. In the preceding year, she had developed prolonged morning stiffness and increasing joint pain, primarily in the metacarpophalangeal joints. Since the onset of her arthritic symptoms, she had also developed an increasing number of deep nodules on the palmar surface of various fingers, with superficial papules over the dorsal surfaces of her fingers, including over the joints. Similar papules recently appeared on her forehead. These lesions were asymptomatic; she denied fever, night sweats, weight loss, or other skin lesions. She had completed 2 courses of prednisone for her arthritis, which reduced joint swelling but did not affect her cutaneous lesions. The lesions had also been treated with “Magic Wart Cream” containing salicylic acid without effect.
Physical examination revealed multiple reddish, 2–4 mm firm papulonodular lesions over the proximal and distal interphalangeal joints of the right hand and dorsal aspects of the fingers bilaterally, and numerous 1–2 mm skin-colored to yellowish, scaly papules along the proximal nailfolds of multiple fingers bilaterally (Figs. 1 and 2). Also present were several reddish, translucent 2 mm papules scattered over the upper forehead near the hairline. Laboratory workup displayed Anti-nuclear antibody positivity at 1:160; Anti-Ro and Anti-La were also positive. Rheumatoid factor was negative. Erythrocyte sedimentation rate and C-reactive protein were normal. X-ray of the hands showed no osseous pathology. Biopsy specimens were obtained from the patient's right dorsal third finger and right fourth finger proximal nailfold (Figs. 3 and 4).- Multicentric reticulohistiocytosis.
- erythema elevatum diutinum
- palisaded neutrophilic and granulomatous dermatitis
A 70-year-old woman with medical history of diabetes mellitus type II, hypertension, hyperlipidemia, and osteoporosis presented to the dermatology clinic 5 years ago for the management of diffuse pruritus, erythroderma, and paresthesia.Complete workup including skin biopsies, polymerase chain reaction for T-cell receptor gene rearrangement, peripheral blood work, flow cytometry, presence of circulating Sézary cells, computerized tomography of the chest, abdomen, and pelvis, and computerized tomography–guided inguinal lymph node biopsy yielded a diagnosis of stage IVA2 (T4, N3, Mx, and B2) Sézary syndrome.
She initially began treatment with photophoresis and romidepsin. For progression of disease, she was transitioned to bexarotene and weekly methotrexate and subsequently was switched to pralatrexate, chlorambucil, and ultimately to vorinostat.
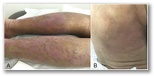
At the present time, in dermatology clinic, she was evaluated for a new diffuse erythematous eruption with eruption of smooth, nonvesicular, papules covering her extremities; some of these papules were coalescing into erythematous thin plaques (Fig. 1A) on top of background of postinflammatory hyperpigmentation and older erythematous patches and thin plaques from her underlying CTCL (Fig. 1B).Few days before the eruption, she had a dermatomal vesicular eruption on the left facial skin that progressed to erythema and crust, which were evident on examination by her medical oncologist.
Clinically, there was a concern for 2 separate contemporary conditions:
- a herpes zoster virus infection on the left face and
- a drug eruption to vorinostat in light of appearance of new erythematous smooth papules. Some of the papules were coalescing and causing thickening of the pre-existing CTCL plaques. Because this was the only medication that had worked well for this patient, it was important to exclude a drug hypersensitivity to vorinostat.
Skin biopsies were obtained from the bilateral extremities
diagnosis?
- ¿?