On Friday 24 February at 12:00 at the Assembly Hall of the Faculty of Psychology of the UV, the neuropsychologist Raul Espert will give a conference where he will explain the roll that plays the discipline of the neuropsychology in the intraoperative brain mapping technique, used to diagnose brain tumours.
22 february 2017
Every year are diagnosed in Spain around 3,000 new cases of primary brain tumours and 14,000 new cases of patients with brain metastasis. Although the complete exeresis of these injuries involves a prognostic factor positive to increase the survival of the patient, it is often hard to obtain because of the difficulty of knowing if the tumour affects areas in which important neuropsychological functions as the language, the movement, the vision, the emotions, etc.
To resolve this difficulty, techniques such as the intraoperative brain mapping with the patient awake have been developed in order to achieve wider resections and with less complications of the brain tumours.
The neuropsychologist and professor of the Department of Psychobiology of the Universitat de València Raul Espert will speak to us about this technique and will give a conference for the students of the Master’s degree in General Health Psychology at the Assembly Hall of the Faculty of Psychology next Friday 24 February from 12:00 in the morning.
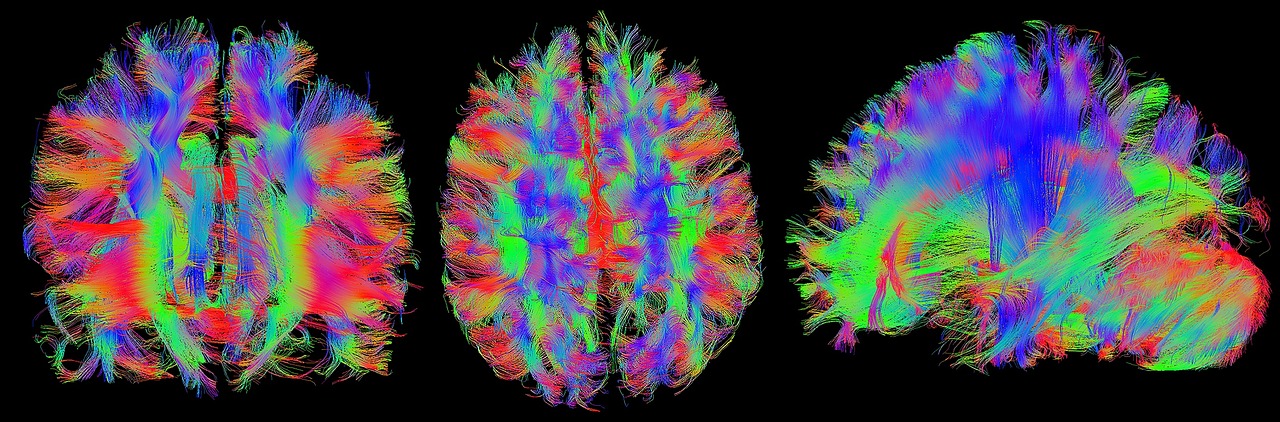
The brain mapping is made through the use of a bipolar stimulator over the brain of the patient awake. The execution of different language, movements, visual fields and emotional expressions tasks are requested to the patient (designed ad hoc and implemented for each patient by neuropsychologists) and the answer during the stimulation is checked both in cortex and subcortically. If an alteration in the language, movement or any of the tested functions is observed, then it is indicated making a personalised brain mapping of areas with functions to preserve. This functional limit of the tumour is compared with the anatomic boundary of tumour obtained through intraoperative ultrasound scan and neuronavigation. This functional information contributes to a greater knowledge of the operational process of the higher cerebral functions and can make possible the execution of wider surgical exeresis with less rate of neurological alterations post-surgery.
The brain mapping is made through the use of a bipolar stimulator over the brain of the patient awake.
The so far used classical functional classification of the brain areas based in post-mortem studies (related to clinical discoveries) are based on the belief that certain functions are invariably attached to determined structures. These studies have been recently proved unreliable because of the great interpersonal variability in the location of functions. This fact has forced the use of brain stimulation techniques like intraoperative brain mapping, which locate each patient’s functional areas accurately.
Given the fact that many of these functions can not be reliably localised before the intervention even with procedures such as functional MRI or DWI (Tractography), their lack of knowledge can affect in two different ways:
1) Reduction of tumour exeresis if during the intervention the resection is stopped intending not to damage areas that are suspected to be eloquent, when in fact if the patient’s brain functional map had been known, the exeresis could have been completed or increased.
2) Increase of the postoperative morbidity caused by an injury during the tumour exeresis of areas that are understood as non-eloquent. This involves the apparition of neurological and cognitive deficits such as language, mobility, visual field, memory disorders alterations, etc. that decrease considerably the life quality of the patient.
Our speaker, the renowned Raul Espert, is a researcher in different financed projects in the field of Psychobiology and clinical and experimental Neuropsychology. Espert, Doctor in Psychology, graduated in these studies in 1987 and, who is in addition, a clinical neuropsychologist in the Neurology Service of the Hospital Clínic Universitari de València, where he has been working since 1999.
He has also been a part of the team of other three hospitals of the Valencian capital city throughout his career: the Hospital Universitario Dr. Peset (from 1993 to 1999), the Hospital Arnau de Vilanova (from 1999 to 2007) and the Hospital Universitario La Fe de Valencia (Neurology Service) since March 2015. All out, Espert has 24 years of experience in neuropsychology in four public hospitals, where he has taken care of more than 14.000 patients with all types of brain damage.
Last year he was awarded with the Premio Neuropsicólogo 2016 del Consorcio de Neuropsicología Clínica and he has authored more than 70 national and international publications, among which there are books, chapters, translations and national and international scientific articles.