Doctoral Thesis - Alba Herrero
clinicaltrials.gov: NCT06032130 / CE UV: 2161984
Introduction
Parkinson's disease (PD) is the second most common neurodegenerative disorder worldwide1. It is a movement disorder characterized by the presence of tremor, rigidity, bradykinesia, and postural instability2. However, 78% of PD patients report visual problems1 such as dry eyes, reduced visual acuity, visual field defects, contrast sensitivity alteration, ocular movement abnormalities, diplopia, convergence insufficiency, color vision impairment, visual hallucinations, and visuospatial orientation problems2-4. In fact, visual dysfunction is one of the initial symptoms of PD5.
A recent study6 has found that dopaminergic neurons affected in PD present physiological dysfunctions but do not die. Currently, PD has no cure, and treatments aim to control symptoms, with earlier detection and administration of treatment being more effective7.
Characterizing the vision of PD patients is proposed because there is a need to further understand how Parkinson's affects vision. Additionally, given the recent understanding that affected dopaminergic neurons do not undergo cell death, implementing a Visual Perceptual Learning (VPL) program in PD patients at an early stage or grouped based on severity and/or duration of the disease is proposed to investigate whether the deterioration of contrast sensitivity experienced by these patients could be slowed or halted.
Visual perceptual learning or VPL is a long-term improvement in visual task performance8, representing any relatively permanent change in perception arising from visual experience9.
Contrast sensitivity (CS) is the ability of the visual system to differentiate an object from its background based on contrast difference, the capacity to detect luminance differences between adjacent areas in an image10.
If results confirm the hypothesis that deterioration can be slowed with therapy, this study would have significant implications for the PD population as it could slow the decline in CS, as demonstrated by several studies11-17.
Consequently, patients would also experience an improvement in their quality of life, as they could continue to perform daily activities affected by visual deterioration such as walking, reading, driving, and cooking18.
This would have a significant impact on society as PD affects many people worldwide. In Europe, the prevalence and incidence rates of PD are estimated at approximately 108-257/100,000 and 11-19/100,000 per year, respectively19.
Moreover, this project would expand scientific knowledge because to date, there is no literature that has evaluated VPL in PD patients. However, there are studies on amblyopia20, Stargardt's disease21, and other neuronal pathologies such as Huntington's disease22.

Objectives
Characterizing the visual problems of the population with Parkinson's Disease (PD) and proposing the potential implementation of a perceptual therapy program in patients with this condition aims to understand all the visual aspects involved in the disease and to slow down the visual deterioration experienced by these patients.
Methodology and Work Plan
Study Type:
This study consists of two distinct phases. The first phase can be classified as an analytical, cross-sectional, prospective, and observational project. Conversely, in the second phase, the study can be classified as analytical, longitudinal, prospective, and experimental.
Description of the Sample:
In the first phase, to characterize the vision of the population with Parkinson's disease, two groups will be recruited. Healthy patients matched for age and gender will serve as the control group, while patients with the disease will form the study group. The control group will be recruited from the University of Valencia community (staff, family members, and La Nau Gran students), and the group with the disease will be recruited from patients and members of the Hospital Arnau de Vilanova and the Parkinson Valencia Association. In both groups, non-probabilistic sampling will be used through invitation to volunteer.
Based on a mathematical formula to estimate a robust sample size without knowing the population size or population standard deviation and setting a confidence level of 95% and a desired estimated precision/error of 0.05: An approximate sample size of 80 Parkinson's patients and 80 age and gender-matched control patients is estimated.
The generic selection criteria for both groups (controls and Parkinson's) are:
- Subjects without ocular or systemic pathologies that may affect the visual system and alter the results
- Subjects without neurodegenerative or neural diseases other than those under study
- Subjects not taking medication that may alter any visual capacity
- Subjects without problems understanding and following the tests
The specific criteria for the control patients are:
- Subjects of similar age and gender as their corresponding Parkinson's patient to ensure age and gender matching in both samples
The specific criteria for patients with Parkinson's are:
- Subjects diagnosed with Parkinson's disease by a neurologist
- Parkinson's patients classified according to the Hoehn & Yahr Scale by a specialist physician
- Patients who have not previously undergone visual therapy programs
- Patients without dementia
In the second phase, to evaluate the effectiveness of a perceptual learning program in patients with Parkinson's disease, the sample will also be divided into two groups: an experimental group and a placebo group. Patients with Parkinson's disease previously measured in the first phase will be randomly assigned to these groups.
Data Collection:
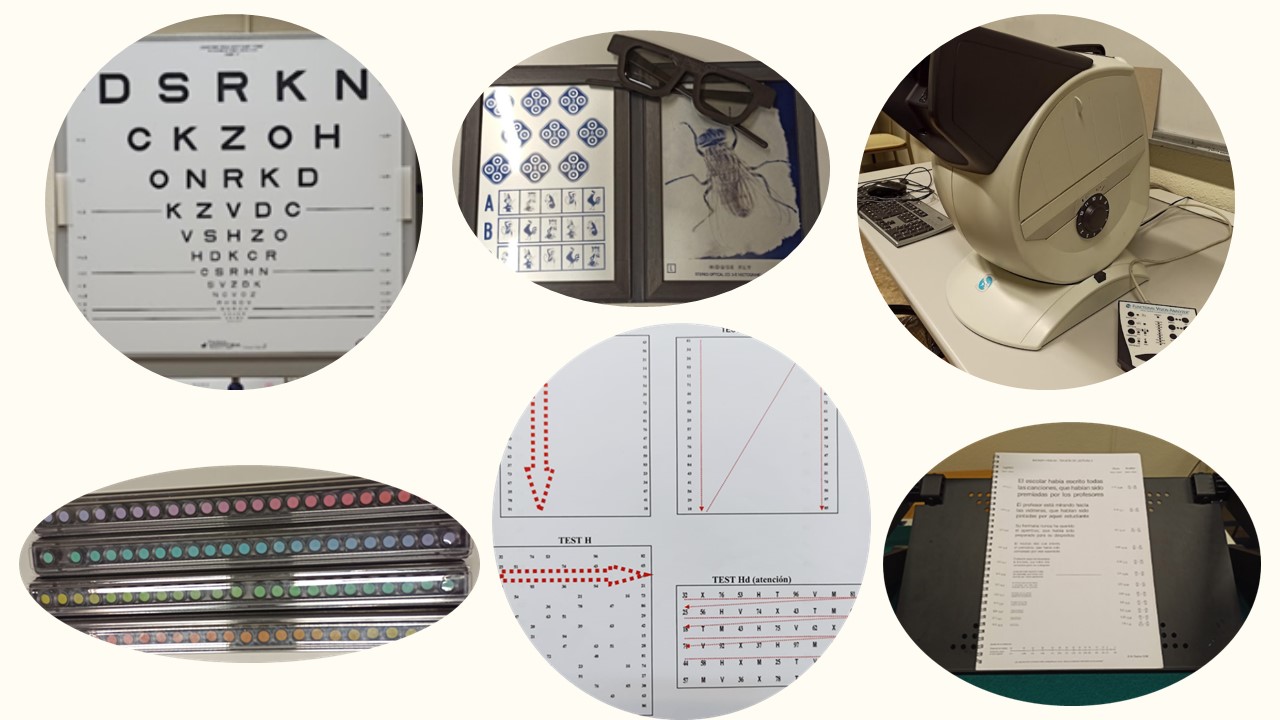
In the first phase, to characterize the vision of the Parkinson's population, all participants, both in the control group and the Parkinson's patient group, underwent a comprehensive optometric examination consisting of the following set of non-invasive clinical tests:
- Anamnesis: gender, date of birth, Hoehn & Yahr classification, medication, systemic, ocular and family history, tobacco, alcohol, drug consumption, coffee intake, physical activity, eye color, and other observations
- Visual acuity and refraction
- Pupilometry under photopic and mesopic conditions and sensory dominance
- Binocularity and depth perception
- Ocular motility and reading speed
- Photopic and mesopic achromatic contrast sensitivity
- Color vision
- Quality of life questionnaire based on visual quality: VFQ-25 questionnaire
The initial tests will be conducted in a session lasting a maximum of one and a half hours. The location for these tests will be at the institution to which each participant belongs.
In the second phase, three visual perceptual exercises of ten minutes each will be performed. These exercises will be conducted every day for eight weeks. Patients will perform them at home using their computer. Contrast sensitivity will be measured every two weeks to assess potential changes and evaluate the effectiveness of the exercises, specifically to determine if there is stabilization of deterioration and/or improvements in contrast sensitivity.
The difference between the control and experimental groups is that while the experimental group will perform visual exercises with Gabor patches of medium-high spatial frequency with decreasing contrast each time, the placebo group will perform them with medium-low spatial frequencies without decreasing contrast.
The control sessions every two weeks are estimated to last approximately half an hour per session.

References
- Yu CY, Lee T, Shariati MA, Santini V, Poston K, Liao YJ. Abnormal eye movement behavior during reading in Parkinson’s disease [Internet]. Vol. 32, Parkinsonism and Related Disorders. Elsevier Ltd; 2016 [cited 2021 Feb 1]. p. 130–2. Available from: https://pubmed.ncbi.nlm.nih.gov/27592009/
- Savitt J, Aouchiche R. Management of Visual Dysfunction in Patients with Parkinson’s Disease. 2020 [cited 2024 Jan 12]; Available from: http://www.nei.nih.gov
- Armstrong RA. Visual Symptoms in Parkinson’s Disease. Parkinsons Dis [Internet]. 2011 [cited 2021 Nov 16];2011. Available from: /pmc/articles/PMC3109513/
- Ekker MS, Janssen S, Seppi K, Poewe W, de Vries NM, Theelen T, et al. Ocular and visual disorders in Parkinson’s disease: Common but frequently overlooked. Parkinsonism Relat Disord. 2017 Jul 1;40:1–10.
- Han G, Han J, Han K, Youn J, Chung TY, Lim DH. Visual Acuity and Development of Parkinson’s Disease: A Nationwide Cohort Study. Mov Disord [Internet]. 2020 Sep 1 [cited 2021 Nov 16];35(9):1532–41. Available from: https://pubmed.ncbi.nlm.nih.gov/32710579/
- González-Rodríguez P, Zampese E, Stout KA, Guzman JN, Ilijic E, Yang B, et al. Disruption of mitochondrial complex I induces progressive parkinsonism. Nature 2021 [Internet]. 2021 Nov 3 [cited 2021 Nov 22];1–7. Available from: https://www.nature.com/articles/s41586-021-04059-0
- Armstrong MJ, Okun MS. Diagnosis and Treatment of Parkinson Disease: A Review. JAMA [Internet]. 2020 Feb 11 [cited 2022 Jan 19];323(6):548–60. Available from: https://pubmed.ncbi.nlm.nih.gov/32044947/
- Sasaki Y, Nanez JE, Watanabe T. Advances in visual perceptual learning and plasticity. Nat Rev Neurosci [Internet]. 2010 Jan [cited 2022 Feb 4];11(1):53–60. Available from: https://pubmed.ncbi.nlm.nih.gov/19953104/
- Fahle M. Perceptual learning: a case for early selection. J Vis [Internet]. 2004 Oct 26 [cited 2022 Feb 5];4(10):879–90. Available from: https://pubmed.ncbi.nlm.nih.gov/15595892/
- Campbell FW, Robson JG. Application of Fourier analysis to the visibility of gratings. J Physiol [Internet]. 1968 Aug 1 [cited 2022 Mar 3];197(3):551–66. Available from: https://pubmed.ncbi.nlm.nih.gov/5666169/
- Bulens C, Meerwaldt JD, Van der Wildt GJ, Van Deursen JBP. Effect of levodopa treatment on contrast sensitivity in Parkinson’s disease. Ann Neurol [Internet]. 1987 [cited 2021 Dec 12];22(3):365–9. Available from: https://pubmed.ncbi.nlm.nih.gov/3674801/
- Pieri V, Diederich NJ, Raman R, Goetz CG. Decreased color discrimination and contrast sensitivity in Parkinson’s disease. J Neurol Sci. 2000 Jan 1;172(1):7–11.
- Diederich NJ, Raman R, Leurgans S, Goetz CG. Progressive worsening of spatial and chromatic processing deficits in Parkinson disease. Arch Neurol [Internet]. 2002 [cited 2021 Nov 23];59(8):1249–52. Available from: https://pubmed.ncbi.nlm.nih.gov/12164720/
- Thomas Hutton JT, Morris JL, Elias JW. Levodopa improves spatial contrast sensitivity in Parkinson’s disease. Arch Neurol [Internet]. 1993 [cited 2021 Nov 23];50(7):721–4. Available from: https://pubmed.ncbi.nlm.nih.gov/8323475/
- Kaur M, Saxena R, Singh D, Behari M, Sharma P, Menon V. Correlation Between Structural and Functional Retinal Changes in Parkinson Disease. J Neuroophthalmol [Internet]. 2015 Sep 29 [cited 2022 Jan 6];35(3):254–8. Available from: https://pubmed.ncbi.nlm.nih.gov/25807477/
- Nowacka B, Lubiński W, Honczarenko K, Potemkowski A, Safranow K. Ophthalmological features of Parkinson disease. Medical Science Monitor. 2014 Nov 11;20:2243–9.
- Price MJ, Feldman RG, Adelberg D, Kayne H. Abnormalities in color vision and contrast sensitivity in Parkinson’s disease. Neurology [Internet]. 1992 Apr [cited 2021 Nov 23];42(4):887–887. Available from: https://www.neurology.org/doi/10.1212/WNL.42.4.887
- Borm CDJM, Visser F, Werkmann M, De Graaf D, Putz D, Seppi K, et al. Seeing ophthalmologic problems in Parkinson disease: Results of a visual impairment questionnaire. Neurology [Internet]. 2020 Apr 7 [cited 2021 Nov 15];94(14):E1539–47. Available from: https://pubmed.ncbi.nlm.nih.gov/32161030/
- Balestrino R, Schapira AHV. Parkinson disease. Eur J Neurol. 2020 Jan 1;27(1):27–42.
- Huang CB, Zhou Y, Lu ZL. Broad bandwidth of perceptual learning in the visual system of adults with anisometropic amblyopia. Proc Natl Acad Sci U S A [Internet]. 2008 Mar 25 [cited 2021 Nov 14];105(10):4068. Available from: /pmc/articles/PMC2268837/
- Sasso P, Silvestri V, Sulfaro M, Scupola A, Fasciani R, Amore F. Perceptual learning in patients with Stargardt disease. Can J Ophthalmol [Internet]. 2019 Dec 1 [cited 2021 Nov 23];54(6):708–16. Available from: https://pubmed.ncbi.nlm.nih.gov/31836104/
- Beste C, Wascher E, Dinse HR, Saft C. Faster perceptual learning through excitotoxic neurodegeneration. Current Biology. 2012 Oct 23;22(20):1914–7.
Parkinson, vision, optometry, visual perceptual learning, clinical psychophysics
- Herrero Gracia, Alba
- PI-Invest Formacio Atraccio Talent
- Diez Ajenjo, Maria Amparo
- PDI-Titular d'Universitat
- Vicedega/Vicedegana / Vicedirector/a Ets
- Hernandez Andres, Rosa Maria
- PDI-Col.laborador/A
- Coordinador/a de Mobilitat
Campus Burjassot/Paterna
C/ Doctor Moliner, 50. 46100 Burjassot (València)
963 544 094
The current research project is part of the Talent Attraction Program 2022, where the principal investigator, Alba Herrero Gracia, has been selected as a beneficiary after a selection process in the competitive call from the Universitat de València. This project is part of the "Talent Attraction 2022" Subprogram of the University of Valencia's Research Grants Program. It adheres to the principles established in the European Charter for Researchers and the Code of Conduct for the Recruitment of Researchers (EEE/2005/251/EC).

This project has established collaboration with the Arnau de Vilanova-Llíria Hospital and with the Parkinson Valencia Association, after being favorably evaluated by the Ethics Committees of these institutions to offer patients and members of these entities the opportunity to participate as volunteers in this project.
Hospital Ethics Approval Number: PI 30_2023
Association Ethics Approval Number: PI14












